Toxoplasmosis Fact Sheet
Authors: Heather Bjerke, Sera Altomari, Christina Broady, Evangelina Burdick, Kayla Munson, Luis Salazar-Vargas, Wendy Zamudio Reyes, Sandra Bushmich
sandra.bushmich@uconn.edu
Reviewer: Elsio Wunder and Emily Reinhardt
Publication July 2024 | EXT073
https://doi.org/10.61899/ucext.v1.073.2024
Introduction
Zoonotic diseases (those that spread from animals to humans) are one of the most common issues of concern worldwide. One Health, a program that
prioritizes the health of humans, animals, and the environment, has been studying how zoonotic diseases are transmitted between animals and humans via
bodily fluids, feces, respiratory droplets, or through inanimate surfaces (known as fomites). Zoonotic diseases may be caused by certain viruses, bacteria, parasites and fungi. This fact sheet is intended for use by those looking for information on Toxoplasmosis, a common protozoan zoonotic disease in the United States.
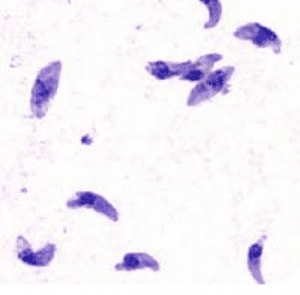
The etiological (origin) agent of toxoplasmosis is a protozoan parasite called Toxoplasma gondii. It is most commonly contracted by eating infected undercooked meat, or through infected cat feces. Domesticated cats and other members of the Felidae family are definitive hosts for Toxoplasma gondii and can transmit the parasite to animals and humans, as well as contaminate food and water resources.
In the United States it is estimated that approximately 11% of the population ages six and older has been infected. However, there are precautions that can be taken to decrease the chances of contracting Toxoplasma gondii, which are detailed in this fact sheet.
Toxoplasmosis can be asymptomatic in those with immune-competent systems, but even among those
individuals it is known to cause flu-like symptoms that can last for months when activated. It can also lay dormant for life, resulting in long-term inapparent infections. Due to how Toxoplasma gondii is transmitted, those who are at higher risk of contracting it are travelers, hunters, and cat owners. Those who may experience greater severity of infection include individuals who have weakened immune systems, infants, and pregnant women as well as their fetuses.
Pathogenesis:
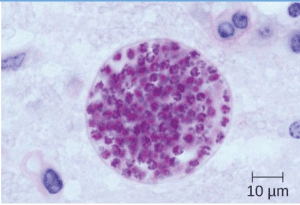
Toxoplasma gondii is transmitted through fecal oocysts, the sporulated form of the parasite. Intermediate hosts such as birds, rodents, pigs, and cows can ingest oocysts in contaminated soil, water, or plants. Humans and other carnivores usually contract the parasite through consumption of infected intermediate hosts, feline feces, soil, food, or water. Women infected during pregnancy can congenitally pass the parasite to their fetuses1.
Symptoms:
Toxoplasmosis can infect both humans and animals. However, there are few tell-tale symptoms since it is typically asymptomatic. An infection can only be truly identified from the detection of antibodies found in blood, that are fighting against the toxoplasmosis parasite.
If symptoms do occur, they may include: swollen lymph glands (especially around the neck), muscle aches, headache, fever, inflammation of the lungs, and inflammation of the eye. Specific symptoms of ocular toxoplasmosis are eye pain, poor vision, and floaters/specks in your vision. ⁸ If the inflamed tissue is left untreated, it can lead to blindness. In most cases where symptoms are present, they appear one to three weeks after being exposed to the parasite and last for about two to four weeks.⁹
A pregnant woman who contracts the toxoplasmosis parasite for the first time, runs the risk of infecting the baby through the placenta. In most cases unborn baby is unaffected. Less commonly, there is a risk of skin rashes, nervous system damage, intellectual disabilities, cerebral calcification (hardening of brain tissue), liver damage, and in rare cases, fetal death. If a newborn is infected, the symptoms are typically a mild sickness.
In cats, if clinical disease is present, the most common symptoms include loss of appetite, lethargy, and fever.
Predisposing/Risk Factors :
While anyone can get be infected with toxoplasmosis, there are several circumstances that can impact the risk of becoming infected and severity of the disease.
- Pregnancy: Being infected with toxoplasmosis when pregnant can be harmful to the unborn child as it can be passed onto the fetus. Infection of the fetus can lead to miscarriage and health problems for the infant later on.4
- Immunocompromised individuals: Those who are at high risk of experiencing greater severity of illness include those with HIV/AIDS, people receiving cancer chemotherapy, and people with organ transplants, due to their weakened immune system.
- Living in a warm, humid environment: Toxoplasma gondii oocysts thrive in warm, humid environments, therefore, there is usually a greater infection rate in these climates. 4
- Owning a cat: Cats are contributors to the transmission of toxoplasmosis through their feces. Cleaning a cat’s litter box, especially if the cat spends time outdoors, can put humans at risk of getting toxoplasmosis. 11
- Gardening: Coming into contact with soil may expose people to areas with contaminated cat feces. 11
- Ingestion of raw/undercooked foods: Transmission can occur by not thoroughly cooking potentially contaminated meat or shellfish. Not properly washing fruits and vegetables can also be a way of being infected. Drinking raw (unpasteurized) goat or other milk or drinking untreated water is dangerous as it may be contaminated.11
TREATMENT:
Treatment for toxoplasmosis depends on the severity of the infection and the individual’s overall health, particularly their immune status.
Immunocompetent Individuals (healthy individuals):
Most healthy people will recover from toxoplasmosis without treatment, as their immune systems can control the infection. If their symptoms are severe, however, individuals may be treated with a combination of two antimicrobials: inhibitors of dihydrofolate reductase (pyrimethamine and trimethoprim), and dihydropteroate synthetase (sulfonamides, such as sulfadiazine, sulfamethoxazole, and sulfadoxine), which block folic acid synthesis. These are prescribed by a healthcare provider as an oral medication.
Immunocompromised Individuals:
For individuals with compromised immune systems, treatment is often necessary to prevent toxoplasmosis from becoming severe and causing complications. It is recommended that individuals with compromised immune systems be treated until their condition improves. Treatment may need to be continued for weeks, or even several months, depending on the severity of the infection. Similar to healthy people, the standard treatment for immunocompromised individuals typically involves a combination of antibiotics, most commonly pyrimethamine, sulfadiazine, and folinic acid, reducing the risk of bone marrow suppression. Alternative treatments consist of atovaquone or clindamycin, with the addition of pyrimethamine.
Pregnant Women, Newborns, and Infants

Pregnant women with toxoplasmosis may be treated with antibiotics to reduce the risk of transmitting the infection to the fetus, although the parasite is not
eliminated completely.
The parasite’s location and ability to remain active within tissue cells makes toxoplasmosis difficult to completely eradicate. Spiramycin, however, is commonly used during pregnancy to reduce the risk of transmission of the parasite to the fetus, especially during early stages of pregnancy. If the fetus is diagnosed with toxoplasmosis, it is most often treated with a combination of antibiotics, specifically: pyrimethamine, sulfadiazine, and folinic acid.
Toxoplasmosis and One Health:
Infected feline hosts without proper treatment can shed Toxoplasma oocysts in their feces for up to three weeks. If left unchecked, domesticated hosts with access to the outdoors increase the risk of transmission as they may end up contaminating nearby soil and water sources. Infected water sources can lead back to local wildlife, and in more severe cases, reach agricultural land and livestock. Other than contact with feline feces, ingestion of raw meats and fish infected with the parasites are also major forms of transmission between animals and humans.
Climate change may also play a role in the overall spread of the parasite.
Changes in migratory patterns caused by ambiguous weather conditions allow infected birds to carry the disease to larger groups of various feline species, poultry intended for human consumption, or bodies of water in different regions. Interestingly, these water sources may already be contaminated due to changes in seasonal precipitation or a rise in temperature, creating the perfect environment for the parasite’s survival. The T. gondii parasite thrives and reproduces in warm, humid environments, areas that are becoming much more accessible to them over time.7
Due to its impact on both warm-blooded animals and surrounding environments, this disease qualifies as a One Health disease. One Health is a task force of concerned scientists throughout the world studying the issues surrounding zoonotic diseases. Approaches include consistent surveillance and data on wildlife and bodies of water at risk, a push for increased screenings for expectant mothers, increased conversation on global environmental change, and putting programs in place to reduce the number of free-roaming domesticated cats.
Prevention and Recommendations:
To reduce risk from food:
- Cook food to safe temperature;
- Use a food thermometer. Color of cooking meat is not a reliable indicator;
- Wash fruits and vegetables;
- Don’t eat raw/undercooked shellfish;
- USDA meat preparation recommendations:
- Poultry: At least 165F
- Ground meat: At least 160F
- Whole cuts of meat: at least 145F To reduce risk from environment
- Avoid consuming untreated water;
- Wear gloves and potentially mouth covering when in contact with outdoor soil/sand that could contain cat feces;
- Cover sandboxes to avoid cat fecal contamination;
- Don’t feed your cat raw or undercooked meat;
- Change cat litter daily, it becomes infectious one to five days after defecation.
If you are pregnant or immunocompromised:
- Avoid changing cat litter, but if you must, wear gloves/face covering;
- Keep cats indoors to lower chances of contact with Toxoplasma;
- Do not handle stray cats, especially kittens;
- Don’t get a new cat while pregnant.
Resources
- Center for Disease Control and Prevention (CDC), “Toxoplasmosis” https://www.cdc.gov/dpdx/toxoplasmosis/index.html
- Pathogenesis image: https://open.oregonstate.education/microbiology/chapter/25-4parasitic-infections-of-the-circulatory-and-lymph atic-systems/
- https://www.mayoclinic.org/diseases-conditions/toxoplasmosis/symptoms-causes/syc-20356249
- https://my.clevelandclinic.org/health/diseases/9756-toxoplasmosis
- https://www.verywellhealth.com/toxoplasmosis-signs-symptoms-and-complications-4160761
- Aguirre, A Alonso et al. “The One Health Approach to Toxoplasmosis: Epidemiology, Control, and Prevention Strategies.” EcoHealth vol. 16,2 (2019): 378-390. doi:10.1007/s10393-019-01405-7
- Yan, Chao et al. “Impact of environmental factors on the emergence, transmission and distribution of Toxoplasma gondii.” Parasites & vectors vol. 9 137. 10 Mar. 2016, doi:10.1186/s13071-016-1432-6
- Park, Young-Hoon, and Ho-Woo Nam. “Clinical Features and Treatment of Ocular Toxoplasmosis.” The Korean Journal of Parasitology, U.S. National Library of Medicine, Aug. 2013.
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/toxoplasmosis
- https://www.cdc.gov/parasites/toxoplasmosis/treatment.html#:~:text=Most%20healthy%20people%20recover%20from,a nd%20sulfadiazine%2C%20plus%20folinic%20acid.
- https://www.cdc.gov/parasites/toxoplasmosis/epi.html
The information in this document is for educational purposes only. The recommendations contained are based on the best available knowledge at the time of publication. Any reference to commercial products, trade or brand names is for information only, and no endorsement or approval is intended. UConn Extension does not guarantee or warrant the standard of any product referenced or imply approval of the product to the exclusion of others which also may be available. The University of Connecticut, UConn Extension, College of Agriculture, Health and Natural Resources is an equal opportunity program provider and employer
